

How To Prevent Cold Sores After Dental Work? (Ultimate Guide)
Have you noticed that every time you go to the dentist, cold sores would start showing up around your mouth? You might brush it off as pure coincidence, but there are actually several reasons why this happens often after getting dental work done.
Cold sores aren’t just embarrassing—these mouth ulcers are painful, too. If getting painful cold sores is a common occurrence for you after you visit the dentist, you might want to go the extra mile and prevent them from showing up.
Today, we’ll take you through how to prevent cold sores after dental work, along with why these blisters show up in the first place. We’ll also share our top tips for caring for these sores if you do end up with them after a trip to the dentist.
Why Do I Keep Getting Cold Sores After Visiting the Dentist?

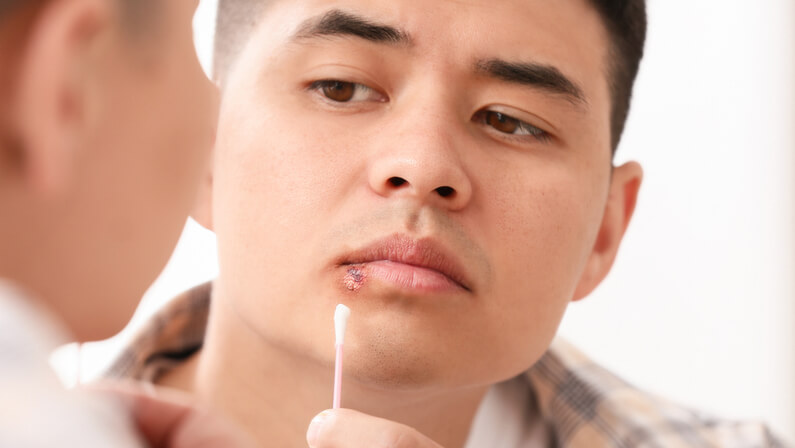
Cold sores, sometimes referred to as fever blisters, are small, red, painful blisters that form around the lips and mouth. They’re caused by a specific herpes simplex virus type called HSV-1—a common kind of herpes that results in infections near the mouth.
Don’t panic—HSV-1 is far from the dreaded genital herpes. Most people will get HSV-1 early in their childhood, maybe even in infancy. That’s why kids often complain about sores when they have them. It is transmitted through saliva or skin-to-skin contact , making it highly contagious.
After you initially catch this virus, it doesn’t go away. It just stays in your body in a dormant state until adulthood. When you have a weak immune system or get stressed , the virus comes alive again, which leads to cold sore outbreaks.
Other symptoms of cold sores from HSV-1 include itching in the mouth area, sore throat, fever, swollen lymph nodes, and feeling like your mouth is drier than usual.
But why do cold sores appear after getting dental work done? The answer is simple—trauma to the mouth.
When you’re in the dentist’s chair getting your teeth done, you might experience trauma to the lips. Small wounds or irritation to the mouth area weaken the tissues there, making it easy for a dormant HSV-1 to reactivate. As a result, you’ll see a fluid-filled blister or two near your mouth.
If you haven’t been infected with HSV-1 before, then you might have gotten the virus from the dental office. The dental clinic, after all, is a healthcare setting where diseases can be transmitted unknowingly.
Tips to Prevent Cold Sores After Dental Work

Want to ensure that you won’t experience those dreaded cold sores and scabs after your trip to the dentist this time around? Here are some ways you can prevent them from popping up around your lips and mouth.
1. Have a strong immune system before your appointment
Whether you haven’t gotten HSV-1 before or have a dormant virus in your body, making sure your body is strong and healthy keeps outbreaks at bay if you catch the virus. A weakened immune system will make you more susceptible to developing cold sores.
So, make sure that when you book your dental appointment, your body feels at its best. If you have a fever or severe headache on the day of your appointment, it might make you more vulnerable to cold sores later on. It might be best to delay your scheduled procedure until you’re better.
To ensure that your immune system is fine before getting dental work done, get a lot of rest and don’t fall victim to stress, as it’s a common trigger of HSV-1 cold sore outbreaks . Eat healthy food and make sure to take your daily dose of vitamin C in the days leading up to your appointment.
2. Ask your doctor for antiviral medicines
Speak with your trusted doctor to tell them about your cold sore situation that happens every time you visit the dentist. Ask them if there are any prescription antiviral medications you can take before going to the dentist to keep it from happening again.
3. Maintain excellent oral hygiene
A clean mouth is a healthy mouth. So, before your appointment, practice the best oral hygiene you can. Always brush your teeth, floss, and gargle with mouthwash to get rid of any bacteria that can make its way to your lips, aggravating any virus.
4. Practice proper lip care to avoid trauma to the lips
Before heading to the dentist, make sure your lips are healthy and moisturized. If your lips are dry, they are more likely to crack while the dentist works on your teeth. As a result, your skin can break, allowing viruses and other bacteria to enter. This can lead to cold sore outbreaks.
You’ll also want to avoid picking at the skin on your lips in the days leading up to your appointment. Any wound or lesion you accidentally cause while doing so can make you vulnerable to cold sores.
If you can, use an SPF-infused lip balm regularly. Not only will this moisturize your lips, but it can also protect them from excess sun exposure—another trigger of cold sores.
What to Do If You Get Cold Sores Anyway

If you still end up getting cold sores after your dental appointment, don’t worry. The best cure for cold sores is to allow the natural healing process to take place. In about 7-10 days, your cold sores will heal completely—as long as you don’t pick at them or try to “pop” the blisters, of course.
Here are some things you should consider doing while you’re nursing your cold sores:
- Keep your lips and mouth area clean. Wash the area with a gentle cleanser or a saline solution to keep the sores from getting infected.
- Use a topical ointment like Zovirax, Valacyclovir, or Acyclovir to treat the blisters and help them calm down. Not only will your sores feel less painful afterward, but this cream can also speed up their healing process.
- Put a cold compress on your blisters, especially when they look and feel inflamed. This can help soothe the pulsating pain from the cold sores.
- If your sores are painful, you can manage the pain at home with over-the-counter pain relievers. For kids in particular, check with your family doctor about what medications they can take to keep the pain of cold sores at bay.
- Avoid hot and spicy foods. Sparkling beverages and acidic, citrusy fruits should also be avoided until the sores get better. These can be irritating to open blisters and can make the pain worse. They may also lead to an infection.
- Practice good hygiene at home. Remember, HSV-1 is highly contagious. Don’t share utensils, glasses, and even towels with other people, lest you pass on the virus to them. Avoid kissing and hugging others to limit the transmission of the virus.
If You Have Cold Sores Before Visiting Your Dentist…
If you have cold sores before your appointment, is it still a good idea to push through with it? Maybe not, but only your dentist will be able to give you sound advice on your situation.
All you have to do is be transparent. Call up your dentist before your schedule and notify them that you’ve noticed some blisters around your mouth. They’ll help you assess your cold sores. If you find that the sores are in their active stage, you will likely be asked to reschedule your dental work.
Dental clinics need to be as safe and sterile as possible to keep every healthcare worker and patient safe and healthy. If you have an active cold sore outbreak, you may compromise the clean, virus-free environment of the dental clinic and pass on the virus to people there.
Plus, if you end up getting your dental work done even with cold sores, there’s a good chance they’ll be even more painful from you opening your mouth a certain way. And if the blister is accidentally punctured, the infection can spread to other areas of your face, like your cheek.
Still not sure if you should book an appointment with your dentist if you have cold sores? Check out what this dentist has to say about the matter so you can weigh the risks before choosing to come in for dental work:
For some people, cold sores are a normal part of getting dental work done. But it doesn’t mean you should just tolerate or be a slave to them. Instead, follow the preventive measures and precautions we listed above to keep them at bay even after a long trip to the dentist’s office.
If you still end up getting cold sores, don’t worry. They will likely clear up in a few days. Just try to keep the area clean and avoid foods that will irritate it.
The best way to avoid getting cold sores altogether after visiting the dentist is to make sure you’re strong and healthy before even booking an appointment. Keep these measures in mind next time you’re anxious about going to the dentist and getting sores again. Your lips will thank you.
Related posts:
- What Is Dental Gold? (Ultimate Guide)
- How Much Does A Dental Check Up Cost? (Ultimate Guide)
- How Many Dental X-rays Are Safe In A Year? (Ultimate Guide)
- How Much Do Dental Crowns Cost? (Your Ultimate Guide)
- What Is A Dental Deep Cleaning? (Ultimate Guide)
- How Much Does A Dental Visit Cost? (Ultimate Guide)
- What Does Restorative Dental Treatment Cover? (Ultimate Guide)
- How Much Does A Dental Filling Cost? (Ultimate Guide)
Similar Posts

Why Do My Teeth Look Bigger? (5 Main Causes)
Many people notice that their teeth look more prominent or larger in size as they get older….

What Is Dental Scaling? (Benefits, Costs & Process)
Dental scaling is a form of dental cleaning of the teeth that’s not dissimilar to the basic…

What Blood Pressure Is Too High For Dental Treatment? (With Tips)
Do you have high blood pressure and need dental treatment? Depending on your blood pressure, you may…

How Long After Dental Implants Can I Eat Normally? (Ultimate Guide)
If you are considering having dental implants, one of the questions on your mind is likely to…

Why Can’t You Eat after Fluoride Toothpaste? (Explained)
Fluoride is a mineral that is commonly found in toothpaste and mouthwash. It is known to help…

11 Dental Diseases That Are Hereditary?
Oral health is determined by a complex combination of genetic, epigenetic, environmental, and behavioral factors. While diet,…

Home > Oral Health
Can You Go to the Dentist with a Cold Sore? Yes, But…
- Written by Dr. Samuel Pacheco H.
- Updated on July 13, 2024
Cold sore? Unless it’s an emergency, the dentist will probably reschedule as cold sores are contagious.

In this article, we’ll talk about the dos and don’ts of visiting the dentist with a cold sore. Read on…
Understanding Cold Sores and Dental Visits
What are cold sores? Cold sores are also known as fever blisters. They are the result of a herpes simplex virus (HVS-1) infection, appearing as one or multiple tiny blisters filled with aqueous fluid.
HSV-1 is a highly infectious virus that hides in the nerves around your mouth and takes advantage of your immune system weakness. Once you are infected with the virus, an active cold sore can show up when you are sick or stressed.
Although cold sores typically manifest on your lips, they can also appear around your mouth, nose, and even inside your oral cavity in severe cases.
Additionally, cold sores are highly contagious and have no definitive cure.
How are cold sores transmitted? Cold sores can spread through close direct contact with the sores or infected saliva. As a result, HSV-1 can be transmitted through daily activities such as sharing utensils or kissing.
Although HSV-1 can be spread even when your sores are not showing up, the risk of contagion is higher when you have an outbreak and the blisters appear.
Importance of dental visits : Cold sores have considerable effects on your oral health. Therefore, regular dental check-ups are essential for maintaining your overall health and spotting early signs of infections or diseases.
During your dental visits, your dentist can detect numerous conditions and address them on time while you receive dental treatments and professional dental cleaning.
Your dentist can detect early signs of herpes virus infections and prescribe medication to prevent virus replication and avoid possible outbreaks.

Implications of Visiting the Dentist with a Cold Sore
- Risk of spreading the virus : Attending your dental visit with an active cold sore increases the risk of virus transmission . Dental work creates tiny droplets that can pass the infection to the dental staff or other patients. Additionally, HVS-1 can survive on surfaces and instruments long enough to infect others, making sterilization and disinfection indispensable in every dental practice to prevent cross-contamination.
- Impact on dental treatment : Certain dental procedures can worsen your cold sore symptoms, such as soreness, pain, and swelling. Also, working during a virus outbreak can lead to discomfort due to your dentist’s manipulation and infection scattering by touching other healthy areas. Therefore, it is typically wise to reschedule your appointment to avoid complications during your treatment and prevent the spread of the virus.
- Precautionary measures for dental staff : Your professional dental team is prepared to deal with numerous infectious diseases. They follow strict hygiene protocols and measures that include wearing gloves, masks, protective glasses, sterile aprons, and keeping a rigorous vaccine schedule. Also, most dental clinics have meticulous disinfection and sterilization protocols with instruments, equipment, and surfaces to prevent common infections . HVS-1 included.
Managing Dental Visits with a Cold Sore
Communicating with the dental office: Your communication with your dental practice is essential. Inform your dentist ahead of time if you have an active cold sore to assess your situation and reschedule your appointment.
With clear dentist-patient communication, you can aid in your treatment plan and help your dental office take the appropriate measures to guarantee your safety and comfort.
Timing of dental visits: Your dentist will probably delay most non-urgent dental appointments until your cold sore healing process is completed. Therefore, understanding how your cold sore evolves is crucial for the correct timing.
Cold sores go through multiple stages, including swelling, blisters, ulcers, scabs, and, finally, a sore and red healed area.
Your cold sore is contagious from blisters to the scab stage. Once you pass that phase, it is safe to attend your dental visits.
Managing cold sore symptoms during the visit : Discuss with your dental team the best action course in case of emergency appointments . Also, use antiviral medications or topical applications to help manage symptoms and reduce the risk of contamination.

You can also apply protective barriers, like cold sore patches, to decrease exposure during your dental procedures.
Additionally, you can take topical anesthetics, anti-inflammatory agents, and analgesics to manage the discomfort and pain that can result from herpes infections.
Conclusion and Additional Tips
Having a healthcare professional’s advice is essential to receive tailored dental attention. Always consult with your dentist to understand your condition and needs and apply the appropriate measures.
With professional guidance, you can receive the best dental care while minimizing risks.
Preventive measures for cold sore management
Maintaining good oral and general hygiene while avoiding sharing personal utensils is a great approach to preventing HSV-1 infections. Keep in mind that most herpes transmissions occur within your close social circle.
If you are already infected by the virus, manage your stress to help prevent outbreaks and be aware of the common symptoms and evolution to prevent infectious stages and protect others.
Besides, follow your healthcare professional instructions and take antiviral medication and analgesics if you frequently experience cold sores to reduce the frequency and severity of the outbreaks.
Final recommendations
Herpes simplex is a highly contagious condition that can go from a mild tingle to blisters around your mouth. Although it does not have a definite cure, it can be manageable and preventable.
In most situations, you should not attend your dental visits with an active cold sore. However, in emergencies, there are steps you can take to manage necessary appointments safely and comfortably.
Remember to prioritize communication with your dental office and follow their recommendations to ensure a safe and effective visit. Avoid masking your lesions or hiding cold sore outbreaks, as it can lead to contagion.
Related Posts
- Teeth Sensitive to Sugar: Why And What to Do About It
- Oral Hygiene: Importance, Practices, and Tips for a Healthy Smile
- Tooth Anatomy: The Structure, Function, and Types of Human Teeth
- Gum Infection Around Dental Crown: How To Treat and Avoid It
- Oral Probiotics: Benefits of Oral Health Pro-Biotics for Teeth and Gums
- Will a Dentist Remove Tonsil Stones?
- Toothpaste: How To Choose the Best Toothpaste for Your Oral Health
- What to Do Before Your Dentist Appointment – Preparing for Dental Visit

A Doctor of Dental Surgery with over 5 years of clinical experience. Additionally, experienced writer and translator with a high proficiency in English and Portuguese.
Latest Articles:

Can You Have Dental Implants With Receding Gums?

Dental Implant Failure: Who is Responsible for Dental Implant Failure?

Braces and Teeth Whitening: Can I Get Teeth Whitening Done While Wearing Braces?
Sign up for our newsletters.
The best of dental tips and news, in your inbox.

Cold Sores and the Dentist
On February 12, 2020 Written and Reviewed by JDC Content Committee

What is a Cold Sore?
Cold sores , also known as fever blisters, are caused by the herpes simplex virus type one (HSV-1). The virus lives in your nerves but damages your skin. It causes sores around the face, usually the lips, that last about one week. In rare cases, cold sores can appear on other parts of your body.
The virus spreads easily by coming in contact with the skin or bodily fluids of an individual with HSV-1. About two-thirds of people carry the HSV-1 infection, but some of them develop cold sores. The combination of a specific genetic component and a trigger (like fever, stress, or too much sun) leads to outbreaks.
Many people experience tingling, burning, or itching sensations prior to an outbreak. The site of the outbreak swells and reddens prior to the appearance of blisters. When the blisters pop, they form cold sores. Eventually, the sores will scab or crust over. Once the crust falls away, the sore is healed.
HSV-1 can be managed but not cured. Prescription antiviral creams can shorten limit the duration of an outbreak, and over-the-counter creams can help with the symptoms.
Though contagious, cold sores are not usually dangerous. However, there are some rare cases that necessitate a visit to a medical professional.
- Your cold sore lasts more than one week without crusting over.
- The cold sore interferes with your ability to speak or swallow.
- Your outbreak is accompanied by a fever.
- You experience a second outbreak of blisters.
What is a Canker Sore?
Canker sores appear on the inside of the mouth and they vary in size. Several factors, like an injury or stress, can cause a canker sore to appear. They vary in size and can occur on the gums, insides of the cheeks or lips, on the tongue, or the roof of the mouth.
It generally takes a week or two for canker sores to heal. Smaller canker sores usually go away on their own with minimal discomfort. Larger canker sores tend to be more painful and may be soothed by over-the-counter creams and gels or prescription treatments, like mouthwashes.
What is the Difference Between Cold Sores and Canker Sores?
Cold sores and canker sores are sometimes used interchangeably because they look and feel alike. However, canker sores and cold sores differ in a few notable ways.
- Cold sores are caused by HSV-1 while canker sores occur due to other conditions.
- The virus that causes cold sores is contagious, but canker sores are not.
- Cold sores appear on the face, usually around the mouth. Canker sores only occur inside the mouth.
Can I Go to the Dentist with a Cold Sore?
Should you go to the dentist with a cold sore? In most cases, no, you should cancel and reschedule your appointment. Since cold sores are caused by a highly contagious virus, there is a risk of spreading it to other people when you have an active outbreak.
It may seem far-fetched that a small sore on your upper lip could cause problems, but until that sore has scabbed and crusted over, the underlying virus is active. Even the most innocent exchange, like touching your mouth and then using a pen or doorknob could pass on the virus.
While you may be afraid to cancel, your dental team will appreciate your concern for their well-being. Contact the office and be honest about your reason for canceling. Keep in mind, cold sores usually last a week or two, so reschedule far enough out to give yourself time to heal.
If you have questions or concerns about cold sores, the team at Jefferson Dental Care can answer them. Contact the clinic nearest you to make an appointment. We’re here to help you keep your mouth healthy!
Our Jefferson Dental Content Committee supports our team by educational and informational articles related to what we do, oral care tips, and current events in our communities.
This blog provides general information and discussions about oral health and related subjects. The information and other content provided in this blog, website or in any linked materials are not intended and should not be considered, or used as a substitute for, dental advice, diagnosis or treatment. This blog does not constitute the practice of any medical, dental or other professional health care advice, diagnosis or treatment. We cannot diagnose conditions, provide second opinions or make specific treatment recommendations through this blog or website.
If you or any other person has an oral health concern, you should consult with your dentist or seek other professional dental treatment immediately. Never disregard professional medical/dental advice or delay in seeking it because of something that you have read on this blog, website or in any linked materials. If you are experiencing a dental emergency, please visit your local Jefferson Dental & Orthodontics office — we accept walk-ins.
Related Stories

Jefferson Dental Sponsors Traders Village
On January 5, 2013

“Jeffy” Motivates Local Kids to Keep Their Teeth Clean
On May 23, 2013

Don’t Wait Till It Hurts: Periodontal Disease
On June 20, 2013
- 717.243.9020
- Appointment Request

- William Noll, DMD
- Devin Caster, DMD, FAGD
- Cali Coble, DMD
- Restorative Team
- Hygiene Team
- Administrative Team
- New Patients
- Accepted Insurance Plans
- Your First Visit
- Pay My Bill
- Financial Information
- Refer A Friend
- Dental Cleanings
- Teeth Whitening
- Gum Disease Treatment
- Smile Restoration
- Cosmetic Dentistry
- Dental Implants
- Root Canal Therapy
- TMJ Treatment
- Dental Sealants
- Crooked Teeth
- Invisalign Treatment
- Orthodontist in Carlisle, PA
- Pediatric Dentistry
- Your Child's First Visit
- Dental X-Rays for Children
- Bruxism in Children
- How Baby Teeth Affect Permanent Teeth
Carlisle's Dental Health Blog

Can I go to the dentist if I have cold sores?
As your stare into the mirror examining the sore on your lip, you realize you have your next cleaning with your dentist coming up. You’ve gotten these sores in the past and know that it’s a cold sore. You also know that the virus that causes cold sores is incredibly contagious, so what do you do? Your smile is important to you and you wouldn’t want to put that at risk. Is a visit worth the potential to spread the virus? The short answer is no, at least not most of the time.
What is a cold sore?
As you may already know, cold sores are a group of tiny, painful blisters that are caused by the herpes simplex virus (HSV). The symptoms you experience are usually the most severe the first time you get a cold sore. Once a cold sore has broken out, your body will usually make antibodies and you might not get another infection. Despite this, it is possible for them to return. They’ll usually appear on the outside of the mouth and lips, but it’s possible for them to show up on the nose and cheeks. Certain things can trigger an outbreak to occur, such as:
- Certain foods
- Sunburn or being in strong sunlight
- Dental work or cosmetic surgery
- Menstruation
For most people having a cold sore outbreak is just an inconvenience and something to be mindful of to prevent the spread. The spread of HSV can occur from kissing someone who has the virus, sharing eating utensils, towels, or razors. Some people with compromised immune systems may need extra care if they develop a cold sore.
Should I keep my appointment?
Given the high transmissibility of HSV, is it wise to go to your dentist? The best thing to do is to call your dentist and ask, but more than likely you’ll be asked to come back at a different time. Even though your dentist will wear gloves while they examine you, it’s still very possible to spread this highly contagious virus. Prior to the healing process that the cold sore goes through, you’re most contagious. Some dentists, however, will begin seeing people with cold sores again after that healing process has started and the sores have begun to scab. Even after that point, some people may experience pain from the dried-out sores. It might be hard to keep your mouth open for extended periods. This is perfectly normal and your dentist would understand if you needed to wait a little longer for the scab to fall off entirely.
Since these sores could easily spread to your dentist or the hygienist, it’s usually best to talk with them to make a plan for rescheduling your appointment once your cold sore has subsided. You want to ensure the safety and health of everyone at your dentist’s office. It’s best to determine where you’re at in the healing process and to give your dentist a call to see what they think.
- Address: 701 S West Street, Carlisle, PA 17013 Get Directions
- Phone: + 1 (717) 243 9020
- Email: [email protected]
We're proud to provide extraordinary dental care in Carlisle , Boiling Springs , & Newville, PA.
WHERE TO BUY
- GET COUPONS

- Abreva Cold Sore Cream
- ABREVA RAPID PAIN RELIEF GEL
- How to Use Abreva Rapid Pain Relief
- ABOUT COLD SORES
- Trigger-Free Summer Vacation Planning
- Visiting the Dentist - Cold Sore Triggers
- What Type of Antiviral Cold Sore Medication Is Right for Me?
- A Parent’s Guide for Managing Teenage Stress
- How Glycerin Helps Cold Sores and Cracked Lips
- FSA or HSA to Purchase Abreva® Products
- GET RID OF COLD SORES
Skip to Content link

- ABREVA PRODUCTS
- MANAGING LIP HEALTH

Dentists and Cold Sores

- DEALING WITH COLD SORES
- STRESS AND COLD SORES
- LIP PROBLEMS
- CAN YOU PUT ALOE VERA ON COLD SORES?
- RECURRING COLD SORES
Back to Managing Your Triggers articles

Going to the Dentist with a Cold Sore
If you suffer from cold sores, you know how stressful and frustrating they can be. Visiting a dentist while you have a cold sore can be worrisome, and can be a trigger for many. Make your dentist an ally and join forces to minimize the chances of an outbreak.
Talk to your dentist
Explain your worries to your dentist. Dental instruments can cause irritation, so be sure your dentist knows that you are prone to cold sores so that he or she can take the proper precautions.
If you already have a cold sore, call your dentist in advance. Some dentists prefer not to treat patients with an active cold sore as it can be painful and cause bleeding and irritation. It’s usually better to reschedule your appointment until the cold sore heals and is no longer infectious.
Apply a cool compress
If you decide to go to the dentist during an outbreak or your cold sore gets painful, apply a cool compress to promote healing. 1 Use a cool, damp cloth to delicately ease the irritability and redness.
- Cold Sores. University of Wisconsin-Madison, University Health Services. Retrieved June 2, 2016, from http://www.uhs.wisc.edu/health-topics/skin/coldsore.shtml
By clicking the link(s) above, you will be taken to an external website that is independently operated and not managed by GSK. GSK assumes no responsibility for the content on the website. If you do not wish to leave this website, do not click on the links above.
PUMP UP YOUR BRAIN

HELP STOP THE SPREAD

KNOCK OUT YOUR CHAPPED LIPS

SHOP FOR ABREVA® NOW

TAKE OUR QUIZ TO DISCOVER YOUR TRIGGERS
TAKE THE QUIZ
- PRIVACY NOTICE
- WASHINGTON CONSUMER HEALTH DATA NOTICE
- TERMS OF USE
This site is intended for US residents only. ©2020-2023 Haleon. All rights reserved.
- Follow us on Twitter (opens new browser tab)
- Watch our videos on YouTube (opens new browser tab)
By clicking the link(s) above, you will be taken to an external website that is independently operated and not managed by Haleon. Haleon assumes no responsibility for the content on the website. If you do not wish to leave this website, do not click on the links above.
Save over $70 with Haleon Huddle
Haleon Huddle unlocks exclusive savings on brands including Abreva, Advil, Sensodyne and more.
*indicates required field.
I consent to the Haleon group of companies and brands (“Haleon”) collecting my Consumer Health Data. Continue reading... I understand that my Consumer Health Data may be used by Haleon as described in our Washington Consumer Health Data Notice , where I can find the categories of data collected, the purposes of collection, and with whom we may share your information. I understand that if I choose not to consent to Haleon’s collection of my Consumer Health Data, I may not be able to receive certain marketing or informational materials or other forms of communication directly from Haleon or participate in surveys and focus groups. I further understand that I may withdraw my consent at any time as described in the Haleon Washington Consumer Health Data Notice or the Haleon Privacy Notice .
I consent to the Haleon group of companies and brands (“Haleon”) sharing my Consumer Health Data with third parties Continue reading... as described in the Washington Consumer Health Data Notice . I understand that I may withdraw my consent at any time as described in the Haleon Washington Consumer Health Data Notice or the Haleon Privacy Notice .
By signing up for Haleon newsletters, you are certifying you are 18 years of age and older.
Check your inbox for a confirmation email from Haleon Huddle to receive coupons!
YOU ARE LEAVING THE SITE
You are now leaving the Abreva.com site and moving to an external website independently operated and not managed by Haleon. Haleon assumes no responsibility for the site. If you do not wish to leave the site, click “Cancel.”
Find a Registered Dental Hygienist
Knowledge network, fact sheet: herpes simplex infection (various intra- or peri-oral infections/manifestations also known as herpetic gingivostomatitis, herpes labialis, herpes simplex labialis, oral herpes, cold sore, and fever blister; finger infection known as herpetic whitlow; caused by herpes simplex virus type 1 [hsv-1] and less commonly by herpes simplex virus type 2 [hsv-2]), is the initiation of non-invasive dental hygiene procedures* contra-indicated, is the initiation of invasive dental hygiene procedures contra-indicated**, oral management implications, oral manifestations, related signs and symptoms, references and sources of more detailed information, is the initiation of non-invasive dental hygiene procedures* contra-indicated.
- Yes, if the patient/client has potentially contagious lesions in or near the mouth, whether from primary herpetic gingivostomatitis or from recurrent oral herpes simplex. Other than oral hygiene instruction, professional care should not be performed until the vesicles/ulcers have completely healed, because of the risk of transmission of the virus to other head and neck areas of the patient/client or to the dental hygienist.
Is medical consult advised?
- Yes, to obtain a definitive diagnosis from a physician or dentist in the case of primary herpetic gingivostomatitis (and associated supportive management) or, in the case of recurrent oral herpes, to potentially obtain antiviral therapy to reduce pain and duration of symptoms.
Is the initiation of invasive dental hygiene procedures contra-indicated?**
- Yes. See above.
Is medical consult advised?
Is medical clearance required?
Is antibiotic prophylaxis required?
Is postponing treatment advised?
- Yes, elective oral care should be postponed until oral and facial lesions of the patient/client have completely healed.
Oral management implications
- Mode of transmission of HSV-1 is primarily via contact with the saliva of carriers, resulting in oral herpes. Transmission may also occur via contact of active cold sores on the lips of carriers or via contact with other active herpetic lesions. Less commonly, according to some sources, herpes virus may also be transmitted via touching objects that are infected with the virus, including infected razors, towels, dishes, and other shared items. Transmission of HSV-2 is usually via sexual contact and causes genital herpes. However, oral-genital, oral-anal or anal-genital contact means that HSV-1 and HSV-2 may be transmitted to various sites, and the historical distinction between the two types of HSV in terms of site of infection is now blurred. After the initial infection, the virus becomes dormant in the sensory ganglia of the face (or genital area); reactivation of the virus causes cold sores of the mouth (or genital sores, if the primary infection was in the genital area).
- Routine barrier infection control measures (i.e., mask, eye protection, and gloves) are essential in reducing the transmission of the herpes simplex virus to oral health care providers.
- Patients/clients with primary herpetic gingivostomatitis (PHGS) should be advised to rest, drink fluids, and eat soft, nutrient-rich foods. Teeth can be cleaned at home with an extra-soft toothbrush if tolerated. Over-the-counter topical anaesthetics and systemic nonsteroidal anti-inflammatory drugs (NSAIDs) can be used to minimize discomfort. However, topical anaesthetics should be used cautiously with children in order not to anaesthetize the throat, which can be distressing.
- Pain associated with oropharyngeal HSV lesions of PHGS can significantly restrict the patient/client’s intake of food, thereby potentially compromising adequate nutrition.
- Even if the dental hygienist has been previously exposed to the herpes virus (which is highly probable) or has had a symptomatic initial infection with or without recurrent lesions, the hygienist can still be inoculated with HSV by inadvertent finger puncture with a virus-contaminated instrument. This can result in herpetic whitlow , which is a potentially recurrent herpetic lesion of the finger that can be very painful and debilitating.
- Patients/clients with recurrent (secondary) oral herpes simplex infections (i.e., cold sores) may be advised to apply ice or a warm washcloth to the lesions for pain relief; wash the blister gently with antiseptic soap and water to reduce potential virus to other body areas; avoid hot beverages, spicy and salty foods, and citrus fruits/juices; gargle with cool water; rinse with salt water; and take a pain reliever such as acetaminophen or ibuprofen. Referral to a physician or dentist is appropriate for consideration of treatment with prescription antiviral agents, with oral medications generally working better than topical formulations. Antiviral medications such as acyclovir, famciclovir, and valacyclovir work best if used during the prodromal (tingling/burning) phase, before any blisters develop. For patients/clients with very frequent recurrences, prophylactic continual use of antivirals may be a consideration.
- Recurrent herpes simplex lesions shed huge amounts of herpes virus, and thus the dental hygienist should not treat the patient/client who has orofacial lesions. Not only are herpetic whitlow lesions a possibility from virus transmission from the patient/client to the dental hygienist, but the virus is also shed in the saliva, and thus spatter during treatment can be hazardous.
- Patients/clients with recurrent oral herpes simplex should be educated about their condition and how to prevent spread of infection. Persons with frequent recurrences are often attuned to the prodromal symptoms, and they should be instructed to reschedule dental hygiene appointments until the episode has run its course.
- The use of sunscreens may reduce the recurrence of herpes labialis in some patients/clients.
- If you, the dental hygienist, have a herpetic whitlow lesion on your hand, you should not engage in patient/client contact until it has completely healed, because you pose an infectious risk to others. Gloves are insufficient protection. Herpetic whitlow of the hand/fingers can last many weeks longer than the usual two weeks or so course of active herpes virus infection in the oral tissue.
- If you, the dental hygienist, have active cold sores (i.e., active primary or recurrent herpetic lesions on the face), you should exercise meticulous infection control (including covering of lesions) when performing procedures involving close proximity to patients/clients. For patients/clients particularly susceptible to infection (e.g., those who are significantly immunocompromised , consideration should be given to deferring elective care until your lesions have healed.
Oral manifestations
- Primary herpetic gingivostomatitis (PHGS) typically occurs following first-time exposure of seronegative persons or those who have not produced adequate antibody response during a previous infection with either of the two HSVs. PHGS typically affects children between the ages of 6 months and 6 years, and may be mild or severe. Many infections are subclinical, with infected persons exhibiting no signs or symptoms. While initial oral infection with HSV-1 usually occurs before the sixth year of life, primary infections in adults are increasingly being reported.
- PHGS is characterized by oral and/or perioral vesiculoulcerative lesions. While herpetic gingivostomatitis is a self-limiting disease, affected persons may experience severe pain that constrains eating and drinking. Symptoms usually appear between 1 to 3 weeks after initial contact with the virus, and may last up to 3 weeks.
- Symptomatic PHGS is usually preceded or accompanied by a burning or tingling sensation at the site of inoculation, cervical and submandibular lymphadenopathy, sore throat, fever, malaise, myalgia, headache, decreased appetite, and pain with swallowing. The characteristic vesicular eruptions may occur on the skin, vermilion border of the lips, or on any mucosal surface intraorally. The discrete, grayish vesicles typically rupture and coalesce within 24 hours to form ulcers with a red, elevated “halo” margin with a depressed gray or yellow central area. The ulcers teem with shedding virus.
- In healthy persons, recovery from primary infection is expected within 7 to 14 days. Only 15% to 40% of seropositive patients/clients go on to experience recurrent mucocutaneous lesions.
- Recurrent (secondary) oral herpetic infection may be triggered by emotional stress, fatigue, fever, sun exposure, onset of menses, illness, and physical trauma. Patients/clients often have prodromal symptoms of pain, burning or tingling at the site where the lesion recurs. Within several hours of the prodrome, vesicles appear, which then become ulcerated and coalesce into a large ulcer or ulcer, typically on the lip or perioral skin. The lesions may be painful, and they crust over as healing occurs. Healing occurs without scarring in about 14 days. Recurrences may be rare, or may occur as often as monthly. Lesions usually recur in the same place on the vermilion border or skin around the face, and recurrent symptoms are usually milder than those associated with the initial episode.
- Recurrent herpetic lesions can occur intraorally — typically on keratinized mucosa of the hard palate or gingiva — as well as on the lips. This distinguishes them from the more commonly occurring aphthous ulcers, which usually appear on the movable mucosa. Dental procedures frequently induce intraoral herpes recurrence on the epithelium adjacent to the teeth.
- In some persons, HSV is present in the oral cavity, even when no lesions are present.
Related signs and symptoms
- Herpes simplex is a viral infection characterized by a localized primary lesion, latency in nerve tissue (e.g., trigeminal, facial, and vagus ganglia), and a tendency to local recurrence. Irrespective of the viral type, HSV primarily affects the mucous membranes and skin. The two causal agents — HSV-1 and HSV-2 — generally produce distinct clinical syndromes, depending on the portal of entry. Either may infect the oral mucosa (oral herpes) or genital tract (genital herpes).
- The prevalence of HSV-1 infection increases gradually from childhood, with up to 90% of the population developing antibodies to HSV-1. Most people in Canada are infected with oral HSV-1 by 20 years of age.
- Unusual manifestations of primary herpetic infection may include non-perioral facial skin (e.g., near the eye). Meningoencephalitis may also occur.
- Herpetic infection of the cornea (i.e., herpetic keratitis) is a serious condition. Recurrences are extremely painful and may last months. Partial loss of sight can occur.
- Neonatal primary infection with HSV can result in fatal generalized infections of newborns infants via viral transmission from the birth canal or, less commonly, via intrauterine transmission. Neonatal risk is elevated if the mother is undergoing primary infection herself.
References and sources of more detailed information
- Laheij AM, Kistler JO, Belibasakis GN, Välimaa H, de Soet JJ; European Oral Microbiology Workshop (EOMW) 2011. Healthcare-associated viral and bacterial infections in dentistry. J Oral Microbiol. 2012;4:10.3402/jom.v4i0.17659. doi:10.3402/jom.v4i0.17659 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3375115/
- Raborn GW and Grace MGA. Recurrent Herpes Simplex Labialis: Selected Therapeutic Options. J Can Dent Assoc 2003;69(8):498-503. http://www.cda-adc.ca/jcda/vol-69/issue-8/498.pdf
- RDH Magazine https://www.rdhmag.com/infection-control/article/16406510/infection-control-and-herpes-simplex
- Today’s RDH https://www.todaysrdh.com/why-hygienists-should-never-treat-patients-with-active-oral-herpes/
- Medline Plus, U.S. National Library of Medicine, National Institutes of Health https://medlineplus.gov/herpessimplex.html
- Bowen DM (ed.) and Pieren JA (ed.). Darby and Walsh Dental Hygiene: Theory and Practice (5 th edition). St. Louis: Elsevier Saunders; 2020.
- Heymann D (ed.). Control of Communicable Disease Manual (20 th edition). Baltimore: American Public Health Association; 2015.
- Little JW, Falace DA, Miller CS and Rhodus NL. Dental Management of the Medically Compromised Patient (9 th edition). St. Louis: Elsevier Mosby; 2018.
- Ibsen OAC and Phelan JA. Oral Pathology For The Dental Hygienist (6 th edition). St. Louis: Saunders Elsevier; 2014.
- Regezi JA, Sciubba JJ, and Jordan RCK. Oral Pathology: Clinical Pathologic Correlations (6 th edition). St. Louis: Elsevier Saunders; 2012.
- Patient Hub
Cold sores and your dental visit

If you have had a cold sore for less than two weeks, please call us to reschedule your appointment. As part of our Infection Prevention and Control measures, our dentists and dental hygiene therapists avoid treating patients with an active cold sore as your lips may be painful and could crack or bleed during treatment. It’s usually better to reschedule your appointment until after this contagious period has passed, to reduce the risk of spreading the virus. A cold sore is most contagious right before the blister forms and while the blister or any scabbing is present, generally around 15 days.
If urgent or emergency dental treatment is required, our dentists will request that your cold sore is fully covered with a cold sore plaster to minimise the risk of cross-infection during your treatment.
After your cold sore goes away, it’s a good idea to replace your toothbrush.
Subscribe to our Newsletter
Sign up for regular updates.

- Our Practice
- Dental Team
- Dental Practice Gallery
- Dental Awards
- Smile Gallery

- General Dentistry
- Advanced Dentistry
- Cosmetic Dentistry
- Dental Implants
- Orthodontics
- Facial Aesthetics
- Lip Enhancement
- UCLan MSc Training Program
- Smile Assessment
- Dentist Payment Plans
- For Professionals
- Dental Hygiene
- Dental Bridges
- White Fillings
- Amalgam Replacement Fillings
- Emergency Dental Service
- Inlays and Onlays
- Mouth Cancer Screening
- Childrens Dentist
- Fluoride Application
- Fissure Sealants
- Dental Trauma
- Missing Teeth
- Tooth Grinding
- Periodontal Treatment
- Surgical & Wisdom
- Dental Veneers
- Boutique Whitening
- Enlighten Whitening
- Smile Makeover
- Composite Bonding
- All-on-Four/All-on-Six
- Implant Retained Dentures
- Single Tooth Dental Implants
- Sinus Lifts for Implants
- Bone Grafting for Implants
- Invisalign™

Can I visit the dentist or hygienist with a cold sore?

Cold sores are small blisters that develop on the lips or around the mouth. They’re caused by the herpes simplex virus and usually clear up without treatment within 7 to 10 days. You may not have any symptoms when you first become infected with the herpes simplex virus.
I’m sure it’ll irk those of you who get coldsores reguarly, that not everyone carries the virus that causes them. I for one, have never had a cold sore, yet my husband gets them very easily, especially when he’s stressed or has a big event coming up. They can also be triggered by illness, exposure to extreme temperatures and UV light (yes, the big, hot, firey ball in the sky can cause them).
Around seven in ten people in the UK have this virus, but only one in three will have any symptoms.
A cold sore usually starts as a tingling or burning sensation around your mouthSmall, painful, fluid-filled blisters then appear, most commonly on the edges of your lower lip. When these blisters burst, the cold sore weeps a highly contagious fluid of viral particles; this stage is very infectious and very painful. After several days a scab will form, protecting the new skin beneath. The scab may dry, crack and bleed, but moisturising may help reduce this. After 9-14 days the cold sore will have healed. The area may be slightly red, but this will soon fade.
Unfortunately, cold sores are infectious and the virus can be passed on to other people by close contact. So no kissing others for starters! It is important to avoid touching your cold sore, because you can pass the virus on to other people’s hands. If you do touch the affected area, you must wash your hands thoroughly with soap and water.
CAN I SEE MY DENTIST/HYGIENIST WITH A COLD SORE?
So the big question here is, can we see you with a cold sore? The short answer is no, we can’t see you within the first 2 weeks of the cold sore appearing. As we work in the area where the infection is (your mouth/lips), it can be really easily spread. Eventhough we have amazing infection control policies in place, even creating an aerosol with a handpiece or the sonic scaler, can be enough to set of a reaction to someone else. Once the virus is in the air, it’s quite difficult to get rid of. And also because your lips may feel sore and could crack of bleed during treatment. This will just prolong the healing process for you as well.
If urgent dental treatment is required ( ie you are in pain and need immediate attention), our dentists will request that your cold sore is protected with a cold sore plaster to minimise the risk of cross-infection during emergency dental treatment.
So, if you do get a cold sore and you have a dental or hygienist appointment arranged, please give us a call on 0121 550 6958 with as much notice as possible, and we can reschedule any non-emergency treatment.
Privacy Overview
- 15580 US Highway 36, Marysville, OH 43040
- Mon - Thu 8:30am - 4:30pm & Fri 8:30am - 2:00pm
- (937) 707-1111
- [email protected]

Mouth Sores at the Corner of the Mouth after Dental Work
- posted by Dr. Doan
- January 14, 2023

A sore on the corner of your mouth could be a result of dental work, or it could simply be a coincidence and non-dental related. It is not uncommon for most people to walk out of a dental appointment feeling fine, but may notice a sore shortly after.
Dental related causes for sore on corner of mouth after dental work
No matter how careful you are, sometimes you can end up with an unintended consequence from a dental procedure. You can count on it being unintentional and the dentist may not even realize it.

Here are some common scenarios which may have caused the sore.
Wisdom tooth cavity filling or extraction
Don’t forget to visit the dentist regularly to ensure that no further dental damage is caused and to maintain a healthy smile. Teeth that far back makes it very difficult for the dentist to get access to it. A person’s mouth is only large enough to open so wide. If you have a small mouth it makes it even harder. Your dentist may have had to stretch your lips out to reach the gum pockets with the drill.
As you can imagine, this situation would apply to any cavity filling on a back tooth and also to taking out a wisdom tooth as well. The same techniques and tools that are used for a root canal on the wisdom tooth can be used on a deep tooth cleaning of a decayed wisdom tooth. This is a common side effect of lip stretching, but it doesn’t have to be that way.
Post operative stress
According to a recent study, canker sores can occur when you are stressed. Even though most people experience some level of dental fear, it’s best to try to address it early on. Situations like adding on a cavity filling or wisdom tooth removal can be quite stressful. This is a common dental problem that many people have, but they don’t know how to fix it or what the problem is. It’s no myth, the root canal is the most feared dental procedure.
Burn from dental drill
You may have been burned from the dentist’s drill during the procedure. You must have been pretty numb to not feel that it was hot. The best way to cool your tooth while drilling a hole is to use water. Sometimes it’s difficult to get enough water sprayed on the tooth. This can cause your lips or tongue to be sore and tender, along with a slight burn.
Eating while you’re still numb
Your dentist appointment will take about an hour, and then it will take 2-3 hours for the numbing to wear off. If you’re feeling hungry, it’s possible that you tried to eat before your numbing wear off and now your lips are chewed up.
Non-dental related causes for sore on corner of mouth
Sometimes the dentist isn’t to blame and whatever went wrong with your mouth could’ve been a pure coincidence. It’s possible that it was a reaction to the oral medication that I took to help reduce any pain from the procedure. It’s really good to be able to answer this question and here are a few reasons as to why there is a sore.

Coincidental cold sore outbreak
If you get frequent canker sores, it may have just decided to appear after your dental appointment. Stress is one of the common causes of canker sores. It can also be caused by a vitamin deficiency. Patients with recurrent aphthous stomatitis often do not consume enough vitamin B12. If this sounds like you, you should have your vitamin levels checked by your primary care doctor. It’s a good idea to do so every year.
Coincidental herpes outbreak
Perhaps it was just a herpes outbreak that coincided with dental work. Of course, a lot of herpes outbreaks are also stress induced. Were you stressed out during the dental procedure? The good news is that there are antiviral treatments for herpes outbreaks. You may take one of these antivrials.
Perhaps it was a combination of dental work and an outbreak of the cold sore virus. You might feel stress during the dental procedure. The majority of herpes outbreaks are also due to stress. Herpes outbreaks are treated by antiviral treatments. The good news is that there are antiviral treatments for herpes outbreaks.
- Famciclovir
- Valacyclovir
To get the prescription for these, you must visit your primary care doctor.
Fungal infection
It’s also possible that you caught a fungal infection after receiving dental work. It’s not uncommon for the mouth to get a fungal infection, so don’t panic. If you have dentures, it’s a good idea to brush them regularly so that they look great and don’t stain or discolor. Patients who wear dentures are often prone to oral candidiasis, which can be treated with anti-fungals.
- Fluconazaole
- Clotrimazole
What should you do about it?
If you happen to get a sore on the corner of your mouth after dental work, there are precautions and treatments that you can do at home.
- Minimize mouth opening. Don’t open your mouth all the way because stretching it will make it worse.
- Lubricate mouth. Apply some vaseline to the corner to keep it moist so it doesn’t crack.
- Stay hydrated. Drrink enough water to prevent the lips from chapping.
- Numbing gel. If it is painful you can apply some anbesol to it.
- Painkillers. You can also take over the counter pain medication like ibuprofen or acetaminophen.
- Rest and nutrition. Your body only heals if it has the nutrients it needs. It also repairs itself while you are sleeping so get some rest.
If it happens to be one of the non-dental related sores, you can take the medications as described above.
How long do the sores on the corner take to heal?
The sore on your mouth could be painful for 1-2 weeks before it goes away. No matter which home treatment you select, you may need to be a bit patient with this process. Be sure to get enough rest and take in nourishing food to give your body the things it needs for healing.
See Dentist For Life
Looking for an experienced and trusted dentist in Marysville , Ohio? Look no further than Dentist For Life! We provide comprehensive dental care for patients of all ages. We take a wide variety of insurance plans and are currently accepting new patients. You can reach us at (937) 707-1111 or schedule your appointment online here .
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Recent Posts
Finding 24-hour emergency tooth extraction services near me, understanding the importance of dental deep cleaning near you, understanding the cost of full mouth dental implants near you, emergency wisdom tooth removal near me – dentist for life, dentist near me accept caresource: accessible dental care for your health needs, opening hours.
We accept most dental insurance and Medicaid plans. New patients are welcome.
Office hours
Monday: 8:30am - 4:30pm Tuesday: 8:30am - 4:30pm Wednesday: 8:30am - 4:30pm Thursday: 8:30am - 4:30pm Friday: 8:30am - 2:00pm Sarturday: Closed Sunday: Closed
- Our dental clinic supports the following languages : English, Vietnamese, Spanish

Copyright © 2022 Dentist For Life. All rights reserved.
- (713) 271-3000
- 9824 Fondren Road Houston, TX 77096
Can I Go to the Dentist With a Cold Sore
- May 11, 2022
- Dental Health
So, can you go to the dentist with a cold sore? The answer is yes, you can go to the dentist, but you will need to be prepared for some possible discomfort .
In this blog post, we’ll talk about how to protect yourself from infecting others and what to expect from your visit. Keep reading for more information!
What Is a Cold Sore?
A cold sore is a small infection on the face, usually around the mouth or nose. Data show that around 80% of the US population has been exposed at some point in their lives, and many people get them several times each year. They are not usually serious, but they can be painful and uncomfortable , which is why you may want to visit the dentist even if you have it.
Although they may be uncomfortable or painful, there are ways that you can protect yourself from the further spread of the infection.
What Are the Causes of Cold Sore?
According to the Mayo Clinic , they’re caused by the herpes simplex virus (HSV). It’s a highly contagious virus that can be passed on through skin contact , kissing , or sharing items like utensils or towels.
Moreover, there are also a number of factors that can contribute to the development, including:
- Stress: Stress can cause the body to release chemicals that can weaken the immune system, making you more susceptible to infection.
- Fever: A fever can also weaken the immune system , putting you at risk of developing a cold sore.
- Diet: Eating a diet that is low in nutrients may also make you more prone to developing cold sores.
- Hormonal changes: This can include things like menstruation , puberty , and pregnancy .
- Weakened immune system: If you have a condition that weakens your immune system, you may be more likely to develop cold sores.
- Certain medications or treatments such as corticosteroids , radiation therapy , or chemotherapy : Can weaken the immune system and make you more susceptible to developing active cold sores.
Does dental work trigger cold sores?
Dental work can trigger cold sores in some people. This is because dental procedures can cause stress and trauma to the lips , which can make the virus more active and cause it to become infected. However, there are steps you can take to protect yourself from spreading the infection and to minimize any discomfort or pain.
These include:
- Taking antiviral medications
- Using a lip balm to protect the skin from irritation
- Avoiding touching other parts of your body after the procedure

What Are the Symptoms of Cold Sore?
The most common sign of a cold sore is a small, fluid-filled blister that appears on the lip or around the mouth. Other symptoms are:
- Pain or burning around the affected area
- Itching or tingling sensations near the blisters
- Sore throat
- Swollen lymph nodes

How Are Cold Sores Treated?
There is no cure for cold sores, but they usually go away on their own within a week or two . There are also ways to manage the symptoms and reduce the duration of the outbreak.
Treatment options include:
- Cold sore creams or ointments: These can help to soothe the pain and speed up the healing process.
- Antiviral medication: This can be prescribed by your doctor and taken orally or applied directly to the cold sore.
- Pain relief medication: This can help to ease any pain associated with the cold sore.

How Are Cold Sores Spread?
Cold sores are spread through direct contact with an infected area, usually through kissing or sharing items like utensils or linens . It’s important to take precautions to prevent the spread of it.
How To Prevent Cold Sore?
There are a number of things you can do to prevent the spread of the virus that causes cold sores, including:
- Avoid close contact with people who have cold sores
- Avoid sharing utensils , towels , or other personal items with someone who has a cold sore
- Wash your hands frequently
- Avoid touching your eyes , nose , or mouth
- Maintain good oral health and observe dental hygiene
- Drink plenty of water
Can I Go to the Dentist With a Cold Sore?

Yes , you can go to the dentist with a cold sore. However, it is important to take some precautions to prevent the spread of infection to others as mentioned above.
Getting a dental treatment with a cold sore can be a little uncomfortable , but it is not impossible .
The first thing you need to do is make sure that you have taken care of it before you go to the dentist.
If your cold sore is in the healing stage , it can be a little painful when the dentist cleans your teeth. You may want to take pain medication before you go in, or talk to your dentist about an antibiotic if you are prone to it.
Another thing you need to think about is protecting yourself against cold sore outbreaks . The best way to protect yourself is by using a lip balm that contains sunscreen and wearing a wide-brimmed hat or sunglasses when you are outdoors.
You should also avoid kissing or sharing utensils with someone who has a cold sore. And, of course, you should always wash your hands before and after touching them.
In general, you should be able to go to the dentist with a cold sore while your teeth hurt without any problems. But it is important to take precautions and work closely with your dentist to make sure that you get the care you need.
So, if you’re feeling under the weather and have a cold sore, don’t panic! You can still go to the dentist, but there are a few things you need to know first. Make sure you protect yourself from infecting others and schedule an appointment with Brownstone Dental today. We’ll take care of everything for you so that your visit goes as smoothly as possible.
- Cosmetic Dentistry
- Dental Health Tips
- General Dentistry
- Oral Hygiene
- Orthodontics
- Pediatric Dentistry
- Uncategorized
Schedule a Consultation
Ready to take the next step toward your dream smile? Contact our friendly team at Brownstone Dental to schedule a consultation. We will be delighted to meet you, discuss your smile goals, and create a customized treatment plan tailored to your needs and preferences.
Patient Reviews
Book An Appointment
- Location 9824 Fondren Road Houston, TX 77096
- Hours of Operation Monday-Friday: 10:00 AM to 6:00 PM Saturday: 9:00 AM to 4:00 PM
- Call Us (713) 271-3000
- Email Us [email protected]
- Hours of Operation Monday-Friday 9:00 AM-6:00 PM Saturday 9:00 AM to 4:00 PM
- Phone (713) 271-3000
- PRIVACY POLICY
Financial Aid Available for Eligible Programs. Registration Now Open.
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
- Skip to footer
- 732-440-4110
ACI Medical & Dental School
A New Beginning, We Change Lives
" * " indicates required fields
Related Posts
- Tips for Stay at Home Moms Going Back to School
- Becoming a Physician’s Assistant in NJ? ACI Can Help!
- Earn Brookdale Medical Terminology Credits at ACI
- The Benefits of Dual Certification at ACI
- Tick Season in New Jersey
Our Results Speak for Themselves
ACI Medical & Dental School students routinely exceed the rigorous standards required by the MSA (Middle States Association of Colleges & Schools).
- 97% Pass Rate on National Credential Exams (7/1/23 – 6/30/24)
- 91% Employment Rate (7/1/22 – 6/30/23)
- 82% Graduation Rate (IPEDS 9/1/20 – 8/31/21)
Accredited By:

Credentialing By:

Approved By:

Contact ACI Medical & Dental School
Contact us today for more information about finding the program that is right for you and enrolling at ACI Medical & Dental School.
ACI Medical & Dental School
- 215 Broad Street Eatontown, NJ 07724
GI Bill® is a registered trademark of the U.S. Department of Veterans Affairs (VA). More information about education benefits offered by VA is available at the official U.S. government Web site at https://www.benefits.va.gov/gibill .
- Testimonials
- Meet Our Staff
- Graduations
- Medical Assistant Certification Program
- Dental Assistant Training Program
- Medical and Dental Administrative Assistant Program
- Secondary Programs
- VA Training Programs
- Federal Direct Loans
- Net Price Calculator
- Program Statistics
- Clery Act Policies
- Campus Crime Statistics
- Accreditation
- Information for High School Seniors
- Why Invest in Education?
- Career Assistance Program
- Employment Opportunities
- Our Employer Partners
- In Demand Careers
- Hire Our Graduates
1311 Jackson Ave Dental
- Apr 26, 2022
Why Is There A Sore On The Corner Of My Mouth After Dental Work?
Updated: Sep 26, 2023
Sores on the corner of your mouth may appear as a result of dental work or it could be purely coincidental and non-dental related. What often happens is that most people walk out of the dental appointment feeling fine but may notice a sore shortly after.

This article will explain what could've possibly caused it and what you can do about it.
Table of Contents :
Dental related causes for sore on corner of mouth after dental work
Wisdom tooth cavity filling or extraction, post operative stress, burn from dental drill, eating while you're still numb, non-dental related causes for sore on corner of mouth, coincidental cold sore outbreak, coincidental herpes outbreak, fungal infection, what should you do about it.
How long for it to heal
That sore on the corner of the mouth could indeed have been an unintended consequence of dental work. It was most likely unintentional and your dentist may not have even realized it during the procedure at all.
Here are some common scenarios which may have caused the sore.
Chances are if it was the very last tooth in your mouth needing treatment such as the wisdom tooth, the sore could've been a result of that. The reason is because when the teeth are that far back, it is difficult for the dentist to get access to it. A person's mouth can only open so wide and if you happen to have a small mouth, it only makes it more difficult. Your dentist may have needed to stretch your lips out to be able to get back there with the drill.
As you can imagine, this situation would apply to any cavity filling on a back tooth and also to taking out a wisdom tooth as well. It is also possible if you needed a deep teeth cleaning on a wisdom tooth as well. The stress from stretching your lips can cause a sore on the corner of your mouth the next day.
Believe it or not, according to this study: canker sores can break out as a result of stress. As you are well aware, anything but a dental cleaning can be a very stressful visit at the dentist.
Most patients have dentophobia and dental anxiety from simply being in the dental chair. If you add on needing a cavity filling or a wisdom tooth removal , the stress levels would be extremely elevated. This stressful hour at the dentist may induce the sore at the corner of your mouth. Let's not forget that the most feared dental procedure of all time, the root canal .
It is also possible that you got burned from the dentist's drill during the procedure. You were probably very numb and couldn't feel that it was hot so you never said anything. Yes, the drill gets very hot and that is the reason why it sprays a lot of water during the entire procedure.
It sprays the water to cool your tooth down and also to keep the drill from over heating. There are times when there is not enough water spraying so it can get hot. This can result in a burn on the corner of your mouth or even leave you with a burnt tongue as well.
The dental appointment took about an hour and then it takes another 2-3 hours for the numbing to wear off. You might've been hungry and tried to eat while you were still numb and accidentally chewed up your lips. That could very well be the reason for the injury to your mouth.
Sometimes it is not your dentist's fault and whatever happened to your mouth could've been a pure coincidence. It just happened to have occurred right after receiving dental treatment. Here are a couple of reasons as to why there is a sore.
If you are someone who gets frequent canker sores, it may have just decided to appear after your dental visit. Canker sores can often be induced by stress or it could be from a vitamin deficiency.
Studies have shown that patients with recurrent aphthous stomatitis typically have a reduced dietary intake of vitamin B12. If this sounds like you, you may want to ask your primary care physician to check your vitamin levels at your next annual check up.
Perhaps it was just a herpes outbreak that coincided with dental work. Of course, a lot of herpes outbreaks are also stress induced. Were you stressed out during the dental procedure? The good news is that there are antiviral treatments for herpes outbreaks. You may take one of these antivirals.
Famciclovir
Valacyclovir
To get the prescription for these, you must visit your primary care doctor.
It is also possible that you caught a fungal infection after receiving dental work. Despite what you think, it is a fairly common occurrence for the mouth to get a fungal infection. Patients who wear dentures are typically more prone to it. The condition is called oral candidiasis and that can be treated with anti-fungals.
Fluconazaole
Clotrimazole
If you happen to get a sore on the corner of your mouth after dental work, there are precautions and treatments that you can do at home.
Minimize mouth opening . Don't open your mouth all the way because stretching it will make it worse.
Lubricate mouth . Apply some vaseline to the corner to keep it moist so it doesn't crack.
Stay hydrated . Drrink enough water to prevent the lips from chapping.
Numbing gel . If it is painful you can apply some anbesol to it.
Painkillers . You can also take over the counter pain medication like ibuprofen or acetaminophen.
Rest and nutrition . Your body only heals if it has the nutrients it needs. It also repairs itself while you are sleeping so get some rest.
If it happens to be one of the non-dental related sores, you can take the medications as described above.
How long do the sores on the corner take to heal?
The sores on the corner of your mouth may take 1-2 weeks for it to fully heal and go away. Some people may take longer if they do not follow any of the precautions or at home treatments listed above. Make sure you get plenty of rest and nutrients so that your body has all of the materials necessary for healing.
Sores on the corner of the mouth that appear shortly after a visit to the dentist may have been treatment related or it could've been non-dental related but coincidentally appeared at the same time. Nonetheless, there are steps that you can take to help the healing process and not delay it. When in doubt, always consult your dentist by making a dental check up appointment.
- Dental Trivia
Recent Posts
Why Dentists Blow Air On Your Teeth During An Exam
White Stringy Stuff in Mouth When I Wake Up
Drinking Alcohol After Wisdom Teeth Removal... Really?

About the author: Dr David Chen, DDS
Hello, I'm Dr Chen and I'm an actively practicing dentist in Long Island City , NY. I graduated from Columbia University College of Dental Medicine in 2016 but prior to going to dental school I was already working in the dental field. It's been more than a decade since I first got to know dentistry and let me tell you, time flies by quickly. Since then I've developed a fondness for writing, which is how this all got started!
Association Memberships:
American Dental Association
New York State Dental Association
Queens Count Dental Society
Medical Disclaimer :
This blog is purely meant for information purposes and should not be used as medical advice. Each situation in your mouth is unique and complex. It is not possible to give advice nor diagnose any oral conditions based on text nor virtual consultations. The best thing to do is to go in person to see your dentist for an examination and consultation so that you can receive the best care possible.
The purpose of all of this oral health information is to encourage you to see your dentist and to inform you of what you may expect during your visit. Due to the unfortunate nature of dentistry, there isn't really any true home remedies that will get rid of dental problems. Roughly 99.99% of them require in-person intervention by a healthcare professional.
Hint: That is the reason why you can't eliminate seeing dentists in your life!
1311 Jackson Ave Long Island City, NY 11101
718-358-3307
Hours : Monday: 9 am-6 pm Tuesday: 9 am -6 pm Wednesday: 9 am -6 pm Thursday: 9 am -6 pm Friday: 9 am -6 pm Saturday: 9 am-3 pm Sunday: Closed
DENTAL SERVICES
Dental Checkup
Teeth Clea ning
Dental Consultation
AI Seco nd Opinion
Teeth Whitening
Deep T eeth Cleaning
Nigh tguard
Botox for TMJ
Tooth Brid ges
Porcelai n Veneers
Invis align
Denta l Implants
Emer gency Dentistry
Tooth Ex traction
Wisdo m Teeth Removal
Denta l Filling
1311 Jackson Ave Dental | SiteMap | Privacy Policy | Ad Disclosure
- Why Choose Legacy Dental
- Meet Our Doctors
- Meet The Team
- Our Technology
- Testimonials
- Smile Gallery
- Membership Plan
- Patient Forms
- Payment Portal
- Dental Crowns
- Porcelain Veneers
- Teeth Whitening
- Smile Makeover
- Dental Implants
- Partial Dentures
- Implant-Retained Dentures
- All on 4 Dental Implants
- Root Canals
- Dental Checkups
- Dental Cleaning
- Family Dentistry
- Tooth Extraction
- Dental Fillings
- Sedation Dentistry
- Wisdom Tooth Extraction
- Broken Dentures
- Mouth Sores
- Temporary Crown
- I NEED A CHECKUP AND CLEANING
- I WANT TO ENHANCE MY SMILE
- I HAVE ONE OR MORE MISSING TEETH
- I AM SCARED OF THE DENTIST
- I AM IN PAIN AND NEED HELP
- I WANT TO GET RID OF CAVITY IN MY TOOTH
- I have headaches or jaw pain
- I have crooked or crowded teeth
- I have bleeding or sore gums
- I don't have dental insurance
- I don't know exactly what I need

How to Treat Cold Sores with Laser Therapy (And Prevent Outbreaks)
Imagine this scenario:
You wake to a tingling, burning sensation on your lower lip and then remember the upcoming (insert important event here) you have this week… Dread and disappoint follow. If you suffer from cold sores, this narrative is all too familiar.
But don’t fret. Our dentists in Salt Lake City have some news to share with you on how to treat and prevent cold sores.
In this blog, we will discuss:
- How to tell if you have a cold sore
- How to prevent cold sores
- How to treat cold sores (spoiler alert – lasers!)
- How to know if you have a cold sore
A cold sore, also known as herpes labialis or a fever blister, is a harmless but irritating fluid-filled blister that goes away in about 10 days from the first symptom (tingling or burning sensation). They appear on the lips and sometimes the skin around the lips.
Herpes labialis, a cold sore virus, is contracted like any other virus. Usually, a person with an active fluid-filled blister exposes a person without the virus. An example of this would be a mother with an active cold sore kissing her child. When first infected, the symptoms mimic the common cold. The virus then can lay dormant in the body until it returns, presenting as sores on the lips.
Canker sore vs. cold sore
Often, cold sores are misidentified as canker sores. A canker sore is a white, yellow, or gray ulcer that occurs inside the mouth. Canker sores are usually caused by trauma (eg., chip to the roof of the mouth) or exposure to certain foods (e.g., citrus juices).
The best way to tell which one you have is, canker sores are inside the mouth, and cold sores are generally outside the mouth.
- What can you do to prevent cold sores?
So, you’ve got the virus already. What can you do to prevent future cold sore outbreaks? Many stimuli can put you at risk for a cold sore outbreak.
Risk factors that can cause an outbreak of cold sores are:
- Wind exposure
- Sun exposure
- Change in weather
Many of these risk factors are difficult to control, particularly stress. For tips on reducing stress, check out our blog post on stress and oral health .
Sun exposure is a big cold sore trigger, so be sure to use protection (sunscreen, hats, etc.) when in the sun to avoid a cold sore outbreak.
- Don’t cause a cold sore reinfection
If you already have an active cold sore blister, take care not to touch it. If you have touched the blister, wash your hands thoroughly. The fluid from the blister can spread and cause other blisters on noninfected areas of the lips, eyes, or fingers.
- How can you treat a cold sore?
For many, the option of waiting 10 days for a cold sore to heal is daunting or simply not possible. Although nothing will take away the cold sore instantly, many remedies help the blister go through the healing process faster.
The most common method to treat cold-sores has been ointments and oral medications, which are antivirals. A newer therapy is treating the sore with a laser.
- Laser therapy
At Legacy Dental , we provide laser therapy on active cold sores. This is best done in the tingling, burning stage of a cold sore. By catching it early, it will help the blister move through the healing phases faster and possibly make it not as big.
Laser therapy is a great cold sore treatment without side effects.
- What to expect with laser therapy
Getting a cold sore lasered is a quick, painless appointment. Our Salt Lake City dentists do not require an appointment for laser treatment of cold sores , and all of our doctors and hygienists are trained in treating cold sores.
After consultation between you and the dentist, you will be given safety glasses to wear. The laser will be used to treat the affected area. It is painless, and most people describe the sensation as feeling nothing or warmth. That’s it!
If cold sores are a recurring ailment for you or your case is extreme, our dentists may suggest medications.
- Now you know: How to avoid and treat cold sores with laser therapy
You can also refer back to this quick infographic outlining what you need to do to prevent and treat cold sores.
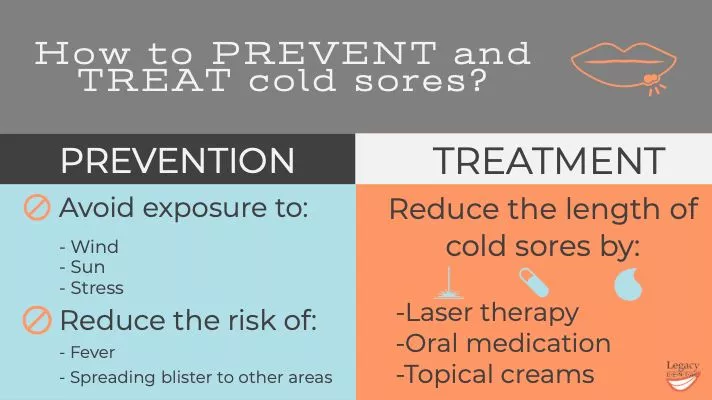
The next time you feel that telltale sign of a cold sore, don’t wait! Call us to treat your cold sore with laser therapy.
If you’re not currently experiencing a cold sore flareup, save our phone number , just in case!
Legacy Dental blog is proudly run by our Salt Lake City dentists team; We share knowledge about general dental care and practices. Apart from running this blog, we offer various dental services such as general dentistry, emergency dentistry , and dental implants for the community in Salt Lake City, Utah
How to reach us in and around Salt Lake City, Utah
Our Doctors Our Services New Patients Smile Gallery Blog Contact Us
South Salt Lake City Millcreek Holladay Murray Wildwood Zions Park
All rights reserved, Copyright 2024 Legacy Dental | Privacy policy | Sitemap Dental Marketing by WEB MARKETING FOR DENTISTS
" * " indicates required fields
5 Stages of Cold Sores and What to Do

In this article
5 Stages of a Cold Sore (How They Form)
Not everyone with cold sores experiences the same set of symptoms or symptoms in the same order.
But there are 5 distinct cold sore stages. A cold sore is contagious from the time you first experience symptoms until it’s completely healed.
Typical cold sore stages include:
Stage 1: Tingling
During this cold sore stage, many people feel an odd sensation where a cold sore develops 12 to 24 hours before they’re noticeable.
Some people describe this sensation as:
- Tingling with numbness
The skin often becomes red, inflamed, and painful as blisters form. It can also become dry and itchy.
People who experience these early symptoms or warning signs of cold sores may never actually have a cold sore outbreak. Applying OTC antiviral ointments for cold sores or taking prescription antiviral medications at this stage may prevent them from forming and improve the healing process.
During first outbreaks, it can take up to 20 days for symptoms to develop after being exposed to the cold sore virus.
Stage 2: Blistering
Tiny, painful, fluid-filled blisters begin to form. Blisters may appear alone or as multiple blisters close together in groups or patches.
At first, a cold sore blister appears clear, then becomes pus-filled and cloudy during this stage. The skin blisters and underneath is typically redder than usual. Do not try to pop, irritate, or break open blisters.
Cold sores typically develop on the lips or around the mouth. But a cold sore can form on the nose, cheeks, and other body parts. Talk to a doctor if cold sores develop on the genitals.
Sores may also develop in the mouth during your first outbreak.
In rare cases, cold sores impact the eyes. Without proper, early treatment, herpes eye infections can affect your eyesight.
Seek immediate medical attention if a cold sore develops near or on the eye, or the eyes become:
- Sensitive to light
Stage 3: Weeping
Cold sore blisters burst and leak, or weep, clear to yellowish-colored fluid for a few days. Sometimes blisters merge before they rupture.
Blisters tend to rupture 2 to 3 days after they develop or 48 hours after warning symptoms develop.
Once they rupture, blisters leave behind shallow, red, exposed, and ulcerated sores. The skin around the sores is often painful, dry, and irritated during this period.
Cold sores are most contagious during the weeping stage. Avoid picking or touching weeping sores to prevent them from worsening, spreading, or becoming infected with bacteria.
Stage 4: Crusting
Like other wounds, after cold sore blisters rupture, they crust and form scabs. Crusting and scabbing typically occur 4 to 5 days after cold sores appear. Scabs may crack or bleed a bit as they heal.
Do not try to pick or pull off scabs or crusting. Applying hydrating creams or ointments can help scabs from becoming too itchy.
Stage 5: Healing
During the final stage of a cold sore, scabs fall or flake off on their own after a few days. The skin underneath scabs tends to be redder, pinker, or more sensitive than normal. It often takes 1 to 3 weeks for sores to heal completely.
Most cold sores don’t leave permanent scars unless they’re severe or extensive. But scabs are often painful and irritating during this stage.
What Causes Cold Sores?
Cold sores are tiny, fluid-filled blisters that usually form on the lips. They are also called fever blisters or oral herpes.
Cold sores are contagious and spread through close contact with bodily fluids or secretions. They are most contagious when the blisters are oozing, but can spread even when invisible.
The herpes simplex virus 1 (HSV-1) causes most cold sores. But the herpes simplex virus 2 (HSV-2) can also cause it. More than 50% of people in the U.S. have the cold sore virus.
After a cold sore heals, the herpes simplex virus becomes dormant (inactive) and lives in nerve cells. Certain factors can trigger the herpes virus to reactivate and cause sores, typically in the same place as before.
Common triggers for cold sores include:
- Sunlight, wind, and cold weather
- Immune changes
- Menstruation
- Dry, damaged, or cracked lips
- Certain foods
- Dental work
- Cosmetic procedures
- Gastrointestinal problems
Common Symptoms
Only around 20 to 40% of people infected with herpes develop cold sores. People usually develop different symptoms depending on whether it’s their first cold sore outbreak.
During your first outbreak, you may experience the following initial symptoms for 1 to 2 weeks:
- A burning sensation in the mouth followed by the formation of painful sores on the lips, gums, tongue, or throat
- Sore throat and pain when swallowing
- Painful gums
- Red or swollen gums
- Muscle aches
- Swollen lymph nodes
During subsequent herpes outbreaks, most people develop painful, hard blisters that ooze clear or yellow fluid once they burst.
How Long Do Cold Sores Last?
Cold sores normally last several days before rupturing and forming a scab. Most cold sore scabs take 1 to 3 weeks to heal completely.
If cold sores are recurring, they are often less severe and only take a week to heal.
When to See a Doctor for a Cold Sore
Most cold sores don’t require medical attention.
Talk to a doctor if you have:
- Cold sores that don’t heal after 2 to 3 weeks
- An immune condition or weakened immune system
- Severe symptoms or frequent, large, or numerous cold sores
- Cold sores on the eyes, genitals, or other body parts
- A fever, spreading redness, or discolored pus
A doctor will typically diagnose a cold sore by looking at it. They may also take a swab of the sore and send it away for testing.
Medical Treatments
There’s no cure for herpes, but some medications can help reduce symptoms and speed up healing.
People with frequent cold sores or a high risk of complications can take antiviral medication routinely or before exposure to triggers. If oral antibiotics are not effective, you can take antiviral medications intravenously (IV).
Home Remedies
Some at-home remedies can reduce cold sore symptoms and improve the healing process.
At-home remedies for cold sores include:
- Applying cold compresses
- Taking oral OTC pain or anti-inflammatory medications, but not aspirin
- Applying OTC topical treatments with numbing agents, like lidocaine, by using a clean Q-tip or cotton swab
- Consuming cold, soft foods and drinks
- Avoiding acidic, salty, or spicy foods
- Applying sunscreen or lip balm with SPF
- Avoiding or limiting exposure to triggers
- Managing stress
- Not touching cold sores
- Applying OTC cold sore patches that protect the skin during healing
- Drinking plenty of fluids to prevent dehydration
- Applying zinc ointments or creams to scabs
- Washing your hands frequently
Some OTC creams and ointments can prevent cold sores if you apply them before they appear (when warning signs develop). They can also improve healing.
Prevention Tips
There are steps you can take to reduce the risk of being infected with the herpes virus. There are also ways to prevent cold sores and recurrent outbreaks.
Common tips include:
- Avoid skin-to-skin or intimate contact with someone with cold sores
- Wash your hands before touching yourself or others when you have cold sores
- Avoid sharing personal items, such as those that touch the skin
- Get enough sleep
- Protect your skin from harsh sun, wind, or cold
- Maintain a healthy, balanced diet
- Avoid contact with sick people
Share this article
Related pages.

Medically Reviewed by Erica Anand

Oral Herpes - Causes, Symptoms & Treatments
Medically Reviewed by Khushbu Gopalakrishnan

Is That a Blood Blister in Your Mouth?

9 Best Cold Sore Treatments for Fast Relief
Medically Reviewed by Nandita Lilly

Mouth Sores
Medically Reviewed by Elena Borrelli

5 Possible Causes of Roof of Mouth Pain & Their Treatments
- American Academy of Dermatology Association “ Cold sores: Overview. ” American Academy of Dermatology Association
- Ceders Sinai “ Cold sores. ” Cedars Sinai
- Cleveland Clinic “ Cold sores. ” Cleveland Clinic
- Johns Hopkins Medicine “ Cold sores .” Johns Hopkins Medicine.
- Mayo Clinic “ Cold sores. ” Mayo Clinic
- National Health Service “ Cold Sores. ” National Health Service.
- Nemours Teens Health “ Cold sores(HSV-1). ” Nemours Teens Health
- StatPearls “ Herpes Simplex Type 1. ” StatPearls
- University of Michigan Health Service “ Cold and canker sores. ” University of Michigan Health Service


Ulcers, cracks and sores – what your mouth can tell you about your health
Senior Lecturer, School of Physiology, Pharmacology and Neuroscience, University of Bristol
Disclosure statement
Dan Baumgardt does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
University of Bristol provides funding as a founding partner of The Conversation UK.
View all partners
The Greek philosopher Zeno of Citium once said that we have two ears and one mouth so that we can listen twice as much as we speak. It’s a sentiment many parents, grandparents – and US TV personality Judge Judy – are fond of repeating. And for good reason too.
But the mouth acts as more than a means of communication, or entry for food and drink. It’s also a way of identifying some internal diseases.
For example, many of us will be familiar with the pesky mouth ulcer . They’re very common and often found on the internal lining of the mouth, the tongue or gingivae – the gums. And by gum are they irritating.
The most common type are aphthous ulcers , round or oval swollen sores, which typically start off yellow in colour before turning grey(ish) later. They often have a red border or “halo” around them.
They don’t last very long and any associated soreness or irritation can be treated with simple painkillers, or by using over-the-counter treatments like sprays or mouthwashes. It’s also a good idea to avoid spicy, salty or sour foods that could be irritating and painful while you have a mouth ulcer.
We’re not sure what causes ulcers but associations have been drawn between physical damage from bite injuries to the inner cheek or tongue. Other possibilities include hormone fluctuation, vitamin and mineral deficiencies and stress.
A few words of caution, though . Minor aphthous ulcers are short-lived and should resolve within a three-week period. Be vigilant for any ulcers that persist longer than three weeks, are near the back of the throat, or are larger than one centimetre in diameter. This is because growing, non-healing lesions can indicate oral cancer . Oral cancer can also present as discoloured patches or lumps in the mouth or throat, causing symptoms like difficulty in swallowing or speaking, and a hoarse voice, among others .
It’s important to get these sorts of symptoms checked urgently by a doctor or dentist. Do be vigilant too for ulcers which bleed, which might suggest either cancer or infection.
Ulcers or sores in the mouth can also be caused by diseases which affect multiple organs. Crohn’s disease and coeliac disease can cause recurrent ulcers – and the patient can notice gastrointestinal symptoms, including abdominal pain and altered bowel habits.
The condition Behcet’s disease can cause painful, swollen joints, and sores which appear not only in the mouth, but also on the genitalia. Ulcers can also be a sign of an impaired immune system.
So, if you’re noticing that you keep getting mouth ulcers – or notice sores elsewhere or other associated symptoms – do make an appointment to see a doctor.
Viral causes
Viruses can cause a wide variety of dots and spots in and around the mouth.
Take the herpes simplex virus, which produces a blistering lesion known as a cold sore , which typically crusts over and heals after a week or two. Avoid skin-to-skin contact (such as kissing) with the sore during this time to prevent transmission of the virus.
Then there is hand, foot and mouth disease , a viral condition particularly seen in children. It causes a rash of sores and blisters affecting the hands, feet and in and around the mouth.
Even the measles virus can trigger a rash inside the mouth known as Koplik spots . Koplik spots are only ever associated with measles. They are white spots that look like grains of sugar or salt on the inside lining of the cheeks. They usually appear before the skin rash erupts, which starts at the head before spreading to the body.
Cracks at the corners
Have you ever noticed soreness or cracks appearing at the corners of your mouth – the areas that are drawn upwards when you smile? That’s angular stomatitis , also known as angular cheilitis or perleche .
It’s a common disorder caused by chapped or dry lips, as a result of viral illness, or from cold weather. But suppose that instead of healing, the cracks continue to hurt, blister or bleed.
The causes of angular stomatitis are extensive , ranging from diseases like Crohn’s and coeliac disease to poorly fitting dentures and infections like thrush. Cracks at the corners of the mouth can also indicate a variety of vitamin and mineral deficiencies too. Iron deficiency is a possibility, or low levels of zinc, folate, and Vitamin B2 (riboflavin) or B12.
So the rule of thumb is that if you notice any sores, ulcers or cracks in and around your mouth that persist beyond a couple of weeks, bleed and don’t seem to heal then do seek medical advice.
- oral cancer

Director of STEM

Community member - Training Delivery and Development Committee (Volunteer part-time)

Chief Executive Officer

Finance Business Partner

Head of Evidence to Action

Canker Sore After Dentist Visit: Why & How To Treat Properly!
Canker sores after dental treatment
Which dental work causes mouth sores.
Aphthous ulcers, also known as canker sores, are a common oral health problem. They appear as round, yellowish or whitish ulcers on the mouth’s lips, cheeks, tongue, and floor. They are often painful and can be single or multiple. Although they are not dangerous and do not cause a fever, they can irritate and make you uncomfortable. If your child develops aphthous ulcers, there is no need to worry – is it possible that you can get one after visiting a dentist?
Canker sores are a common problem that can occur after dental treatment. They are small, painful ulcers that can make it difficult to eat or speak. While there is no cure for canker sores , there are steps that you can take to help reduce their severity and shorten the duration of the outbreak.
If you experience canker sores after dental treatment, here are a few things that you can do to help relieve the pain and speed healing:
- Apply ice or a cold pack to the sore for 10-15 minutes daily. This will help reduce inflammation and pain.
- Take over-the-counter pain medications such as ibuprofen or acetaminophen to help relieve pain.
- Rinse your mouth with salt water several times a day to help keep the area clean and help promote healing.
- Avoid eating acidic or spicy foods, as these can aggravate the sore and prolong the healing process.
- If necessary, you may also want to consider taking an over-the-counter oral steroid medication to help reduce inflammation and speed healing.
If you experience canker sores after dental treatment, there are a few things that you can do to help reduce their severity and shorten the duration of the outbreak. Following these tips can help keep your mouth healthy and pain-free.
Is it common to get a canker sore after dental work?
Canker sores are a common problem that can occur after dental treatment. They are small, painful ulcers that can make it difficult to eat or speak. While there is no cure for canker sores, there are steps that you can take to help reduce their severity and shorten the duration of the outbreak.

Any dental work can potentially cause canker sores.
Common triggers include:
- tooth extractions
- dental cleaning
- dental injection (novocaine shot)
- wisdom tooth removal
If you have a canker sore, you may notice a tingling or burning sensation a day or two before the sore appears. The sore is usually round or oval and white or yellow with a red border. Canker sores typically heal within two to three weeks without treatment. However, they can be painful and make it difficult to eat or drink.

How To Fix Receding Gums At Home & Other Possible Treatments!

Should You Floss Teeth Twice A Day? Can You Floss Too Much?

Why Do I Metabolize Anesthesia Faster? Discover the Surprising Reasons

Bit Lip Healing: Top Tips and Remedies for Quick Recovery

Can a Tooth Grow Back After Extraction? Discover the Truth

How to Strengthen Loose Teeth Naturally: Top Tips for a Healthy Smile
Privacy Policy
- Orthodontics Niche Guest Post Offer: Write for Us and Share Your Expertise
- Write for Us in the Dentistry Niche: Guest Post Offer

Compare items
- Total ( 0 )
What Dentists Can Tell About You Just By Looking In Your Mouth
Senior Reporter, HuffPost Life

When you go to the dentist, you’re likely focused on matters like cavities and gum health. But dental experts can detect a lot more from your exam.
“A lot about someone’s overall health can be observed just by looking in their mouth,” Dr. Kami Hoss , a dentist and author of “If Your Mouth Could Talk,” told HuffPost. “In fact, over 100 systemic conditions and many medications can have oral manifestations. This means that what happens in the mouth can often be a window into broader health issues, helping to identify problems before they escalate.”
Because the mouth is considered the “gateway” to the body, it can also be the origin of problems in many different bodily systems.
The mouth’s microbes “can enter the bloodstream through bleeding gums or open root canals and travel to other parts of the body, causing infections or inflammation,” Hoss noted.
That’s why routine dental checkups are so important.
“A comprehensive oral examination can provide valuable insights into a person’s overall health and lifestyle habits, helping dental professionals identify potential issues and provide appropriate care and recommendations,” said cosmetic dentist Dr. Michael J. Wei .
So what exactly can a dentist infer about you from the state of your mouth? We asked some professionals to share what they’ve seen.
If You Floss Regularly... Or Rarely
“Unfortunately, dentists can’t be fooled into thinking you floss regularly if you floss just right before your visit,” said Dr. Erin Fraundorf , an orthodontist and founder of BOCA Orthodontic + Whitening Studio. “Gum tissue that is not flossed regularly looks red, inflamed and may bleed.”
She noted that healthy gums are pink and smooth with a “knife-edge” instead of puffy.
“As soon as your dentist sees your mouth and the color and texture of your gums, they can tell you have gum disease,” Fraundorf said.
If Your Diet Is High In Certain Foods And Drinks
“Erosion and decay on teeth can reveal a lot about someone’s diet, with high consumption of sugary foods and beverages typically leading to cavities, while acidic foods and drinks, like citrus and soda, can cause enamel erosion,” said cosmetic dentist Dr. Kevin Sands .
Highly acidic and sugary foods and drinks can also contribute to gum disease.
“If you are a big tea or coffee drinker, you will more likely have dark stains,” Fraundorf added.
If You Have Diabetes
People with diabetes often have inflamed gums.
“Imbalances in sugar may also result in a rapid change in the health of your gums, showing up as increased swelling, bleeding and sensitivity,” Fraundorf said. “Diabetic patients have a higher prevalence of gum disease.”
Additionally, “fruity” breath can be a sign of uncontrolled diabetes, so patients should seek medical attention if they experience this phenomenon.
If You Bite Your Nails Or Suck Your Thumb
“Without glancing at your nails, a dentist may be able to detect if you bite your nails ― or bite on other items, like pen caps or bottle caps,” Fraundorf said, noting that the stress on your teeth can cause chipping and other wear and tear.
Dentists can also tell if you suck your thumb or did a lot in the past (beyond early childhood).
“Thumb-sucking may significantly alter not only a patient’s teeth but their jaws,” Fraundorf explained. “These signs include protruding upper front teeth with spacing, tucked back lower front teeth with crowding, a narrow upper jaw and an anterior open bite ― a lack of vertical overlap between the upper and lower front teeth.”
Similarly, tongue thrust can result in an anterior open bite, but generally both the upper and lower teeth will have protrusion and spacing, she added.
If You’re Deficient In Vitamins And Minerals
“Deficiencies in essential nutrients can impact the health of the teeth and gums,” Wei said.
Dry mouth, sores and bleeding gums are common manifestations, as well as changes in the tongue.
“Being deficient in vitamins and minerals may result in many oral conditions, like increased infections, burning tongue syndrome, sore tongue, cracked lips, tissue sloughing, delayed healing, bone infections, and gums that bleed easily,” Fraundorf said. “When patients are deficient in iron, their gum tissues can lose some of the red hues and turn pale pink or even white. Light pink, pale gums can be a sign of anemia.”

If You’re Right- Or Left-Handed
“It’s pretty wild, but we can often tell if you’re left- or right-handed ― or at least we can tell if you brush with your right or left hand,” Fraundorf said.
Right-handed patients typically don’t brush their upper right teeth as well as they do their left side. The reverse is true for lefties.
“This leaves the gums slightly more puffy and red in addition to more plaque retention on these teeth,” Fraundorf explained.
If You’ve Struggled With An Eating Disorder
Dentists can also see the effects of disordered eating in their patients.
“Patients with eating disorders, specifically bulimia, will typically show enamel erosion or breakdown of enamel,” Fraundorf said. “Specifically, we see erosion almost exclusively on the tongue side of your teeth from the stomach acid that comes up into the oral cavity.”
If You Have A Gastrointestinal Issue
Instead of disordered eating, this kind of erosion might also indicate a GI problem.
“Persistent bad breath might indicate gastrointestinal issues such as GERD, where stomach acid damages teeth and soft tissues,” Hoss said. “The mouth can also reveal early signs of certain gastrointestinal diseases. Crohn’s disease can cause swelling of the gums and mouth ulcers before any intestinal symptoms appear. Oral manifestations like these can be critical for early diagnosis and treatment of serious conditions.”
If You’re Exhibiting Signs Of Certain Cancers
“The mouth can also reveal early signs of certain cancers,” Hoss said. “For instance, signs of leukemia may present as gum overgrowth and bleeding. Oral manifestations like these can be critical for early diagnosis and treatment of serious conditions.”
Oral cancer can also manifest in the mouth with visible oral lesions or growths.
“Signs of oral cancer include unexplained bleeding in the mouth, patches (red, white or spotted), changes in your bite, or areas in the mouth that are eroded, lumpy or swollen,” Fraundorf said. “The patient should then visit an oral surgeon for a consultation and biopsy of any suspicious tissue.”
If You’re Pregnant
“Some women may develop a deep red lump on their gums called a pregnancy tumor or pyogenic granuloma ― a totally benign tumor that will resolve once pregnancy is over,” Fraundorf said.
She noted that pregnancy also commonly leads to the development of gingivitis due to increased progesterone, which facilitates the growth of bacteria.
If You Have An Autoimmune Disease
“Dentists are the first line of defense in detecting system diseases and nutrition deficiencies because some of these diseases and deficiencies have oral manifestations,” said Dr. Jarrett L. Manning , founder of JLM Dental Studio. “This means the disease process may present as abnormal mouth lesions that dentists are trained to detect.”
While dentists check for gum health, tooth conditions and overall mouth hygiene, Manning emphasized that any dental checkups are also important because “any lesion, sore, or patch in the mouth can tell another story and give us insight to a deeper issue.”
The list of potential deeper issues includes various autoimmune diseases and other inflammatory conditions.
“Red spots and sores may be signs of lupus and Crohn’s disease, and white spots in the mouth may be linked to lichen planus,” Fraundorf said. “These spots may be tender or painful and may lead to mouth ulcers.”
If You’re Experiencing Kidney, Liver Or Bone Problems
“Bad ‘fishy’ breath and chronic dry mouth may be signs of kidney problems,” Fraundorf said.
She noted that fishy breath may also indicate liver failure. Your dental appointment might also lead to the discovery of bone issues.
“A dental examination with X-rays can reveal bone loss and may lead to an early diagnosis of osteoporosis ― a disease of the bones which results in bone loss and an increase in brittleness,” Fraundorf said.

If You’re Dealing With Stress Or Sleep Issues
“Clenching or grinding of teeth, also known as bruxism, can be a sign of stress or anxiety, which can have detrimental effects on oral health,” Fraundorf said.
Dentists can spot this sort of excess wear on the biting surfaces of teeth.
“Teeth grinding and redness of gum tissue and the throat may also be signs of sleep apnea ― a serious condition which limits the amount of oxygen a person gets during sleep,” Fraundorf added.
If You Have HIV
“You can see if someone has HIV by identifying specific lesions called Kaposi’s sarcoma that are common in uncontrolled HIV cases and have a distinct visual appearance,” said Dr. Ilona Casellini , founder of Swiss Quality Smile.
People with HIV may also experience chronic dry mouth, canker sores and hairy leukoplakia, which presents as white patches on the tongue.
“Oral yeast infections can be a symptom of HIV in young patients who seem to otherwise present as healthy,” Fraundorf noted.
If You Smoke
“Lifestyle choices leave distinct signs in the mouth too,” Sands said. “Smoking or using tobacco products can cause stained teeth, gum disease, and a higher risk of oral cancers.”
Drug use can also have a noticeable impact on the teeth and other parts of the mouth.
If You Struggle With Alcohol Misuse
“Alcoholics often have inflamed gums and breath that smells of alcohol,” Casellini noted.
Alcohol tends to dry out the mouth, making people with drinking issues more susceptible to cavities.
If Your Oral Hygiene Habits Are Inconsistent Or Insufficient
“The presence of plaque, tartar, and gum inflammation often indicates a person’s oral hygiene routine, suggesting inconsistent or insufficient oral care if these issues are present,” Sands said.
He emphasized that maintaining oral health is crucial not just for a beautiful smile but also for overall well-being. Awareness and proactive care can significantly impact someone’s quality of life.
Examining the mouth might also reveal signs of mental impairment or decline, particularly for older patients.
“Patients with cognitive disorders such as dementia or Alzheimer’s often exhibit poor oral hygiene,” Casellini noted. “They might forget to brush or have lost manual dexterity.”
From Our Partner
Huffpost shopping’s best finds, more in life.

COMMENTS
To ensure that your immune system is fine before getting dental work done, get a lot of rest and don't fall victim to stress, as it's a common trigger of HSV-1 cold sore outbreaks. Eat healthy food and make sure to take your daily dose of vitamin C in the days leading up to your appointment. 2. Ask your doctor for antiviral medicines.
Cold sore: Yes, patients with a history of cold sores often do not tolerate manipulation of oral soft tissues, particularly the lips, cheeks. What We Treat. ... When I visit the dentist 90% of the time I get a cold sore outbreak (I have been having cold sores since I was 5 Years old). My last outbreak was 4 days after dental cleaning.
The key is to call your dentist immediately: that is, as soon as you start to feel the flare up. At this point, the cold sore blister isn't in its contagious stage, so it's safe for your dentist to see you. It's also the key time to use a dental laser on your lip, to interfere with the viral flare-up, so that the blister goes away in half ...
Cold sores go through multiple stages, including swelling, blisters, ulcers, scabs, and, finally, a sore and red healed area. Your cold sore is contagious from blisters to the scab stage. Once you pass that phase, it is safe to attend your dental visits. Managing cold sore symptoms during the visit: Discuss with your dental team the best action ...
Patients who present with cold sores, especially in the vesicle stage, should be advised of the potential risk of spreading the virus to the nose or eyes if oral tissues are manipulated. Many dental practices have policies on treating (or not treating) patients with active cold sores. It is up to each oral health professional to decide when it ...
Cold sores, also known as fever blisters, are caused by the herpes simplex virus type one (HSV-1). The virus lives in your nerves but damages your skin. It causes sores around the face, usually the lips, that last about one week. In rare cases, cold sores can appear on other parts of your body. The virus spreads easily by coming in contact with ...
Some dentists, however, will begin seeing people with cold sores again after that healing process has started and the sores have begun to scab. Even after that point, some people may experience pain from the dried-out sores. It might be hard to keep your mouth open for extended periods. This is perfectly normal and your dentist would understand ...
Apply a cool compress. If you decide to go to the dentist during an outbreak or your cold sore gets painful, apply a cool compress to promote healing. 1 Use a cool, damp cloth to delicately ease the irritability and redness. Cold Sores. University of Wisconsin-Madison, University Health Services.
Patients/clients with recurrent (secondary) oral herpes simplex infections (i.e., cold sores) may be advised to apply ice or a warm washcloth to the lesions for pain relief; wash the blister gently with antiseptic soap and water to reduce potential virus to other body areas; avoid hot beverages, spicy and salty foods, and citrus fruits/juices ...
A cold sore is most contagious right before the blister forms and while the blister or any scabbing is present, generally around 15 days. If urgent or emergency dental treatment is required, our dentists will request that your cold sore is fully covered with a cold sore plaster to minimise the risk of cross-infection during your treatment ...
After several days a scab will form, protecting the new skin beneath. The scab may dry, crack and bleed, but moisturising may help reduce this. After 9-14 days the cold sore will have healed. The area may be slightly red, but this will soon fade. Unfortunately, cold sores are infectious and the virus can be passed on to other people by close ...
A cold sore is a small, painful, raised area of small, fluid-filled blisters. They usually happen where the lip joins the surrounding skin. The blisters are painful and dry up to make a yellow crust which gradually heals in a few days. Cold sores are usually found on the lips but you can get them in other places, such as in the nostrils, on the ...
Coincidental cold sore outbreak. If you get frequent canker sores, it may have just decided to appear after your dental appointment. Stress is one of the common causes of canker sores. It can also be caused by a vitamin deficiency. Patients with recurrent aphthous stomatitis often do not consume enough vitamin B12.
Yes, you can go to the dentist with a cold sore. However, it is important to take some precautions to prevent the spread of infection to others as mentioned above. Getting a dental treatment with a cold sore can be a little uncomfortable, but it is not impossible. The first thing you need to do is make sure that you have taken care of it before ...
Keep the dentist in the loop. Some dentists do not want to see patients with cold sore scabs. Even though these sores are not nearly as contagious at this point, they are still slightly contagious. Some dentists will want to reschedule the dental checkup. Contact the dentist at least 24 hours in advance to talk about the situation.
Should you visit the dentist with a cold sore? What is a cold sore? A cold sore is a small, painful, raised area of small, fluid-filled blisters. They usually happen where the lip joins the surrounding skin. The blisters are painful and dry up to make a yellow crust which gradually heals in a few days. Cold sores are usually found on the lips ...
Cold sores and fever blisters are caused by herpes simplex virus type 1 (HSV-1). This virus is passed from person to person by saliva (either directly, or by drinking from the same glass or cup) or by skin contact. Cold sores usually appear as clusters of tiny blisters on the lip. About 8 out of 10 people have the virus that causes cold sores.
Sores on the corner of your mouth may appear as a result of dental work or it could be purely coincidental and non-dental related. What often happens is that most people walk out of the dental appointment feeling fine but may notice a sore shortly after. This article will explain what could've possibly caused it and what you can do about it.Table of Contents: • Dental related causes for sore ...
Cold sore therapy. What wonderful information was presented in the August JADA For the Patient page (Mark A. Common Oral Sores and Infections. JADA. 2020;151 [8]:640). Very helpful. It was also great to see that the information was given with permission for print and reproduction. Although the information on cold sores was perhaps very adequate ...
At Legacy Dental, we provide laser therapy on active cold sores. This is best done in the tingling, burning stage of a cold sore. By catching it early, it will help the blister move through the healing phases faster and possibly make it not as big. Laser therapy is a great cold sore treatment without side effects.
Stage 4: Crusting. Like other wounds, after cold sore blisters rupture, they crust and form scabs. Crusting and scabbing typically occur 4 to 5 days after cold sores appear. Scabs may crack or bleed a bit as they heal. Do not try to pick or pull off scabs or crusting.
Immediately after, another cold sore appeared at the spot where the dentist was pulling my lip. Same thing with the third. I just had my third filling done and two days after my appointment I have a cold sore again at the spot where my lip corner was being pulled on.
From cold sores to oral cancer ... It's important to get these sorts of symptoms checked urgently by a doctor or dentist. Do be vigilant too for ulcers which bleed, which might suggest either ...
If you experience canker sores after dental treatment, here are a few things that you can do to help relieve the pain and speed healing: Apply ice or a cold pack to the sore for 10-15 minutes daily. This will help reduce inflammation and pain. Take over-the-counter pain medications such as ibuprofen or acetaminophen to help relieve pain.
Dry mouth, sores and bleeding gums are common manifestations, as well as changes in the tongue. "Being deficient in vitamins and minerals may result in many oral conditions, like increased infections, burning tongue syndrome, sore tongue, cracked lips, tissue sloughing, delayed healing, bone infections, and gums that bleed easily ...
Hop on for our weekly Q&A where I answer any dental or homesteading question!